Vaginal Prolapse – Symptoms, Diagnosis, and Treatment
Vaginal prolapse is a general term for a group of specific disorders that are, simply, hernias of the vagina. A hernia is what happens when tissues and organs pass into/through a space that they wouldn’t normally move into/through. This space can occur naturally (like the vaginal opening) or can be created quickly (with surgery or trauma) or slowly (with chronic pressure).
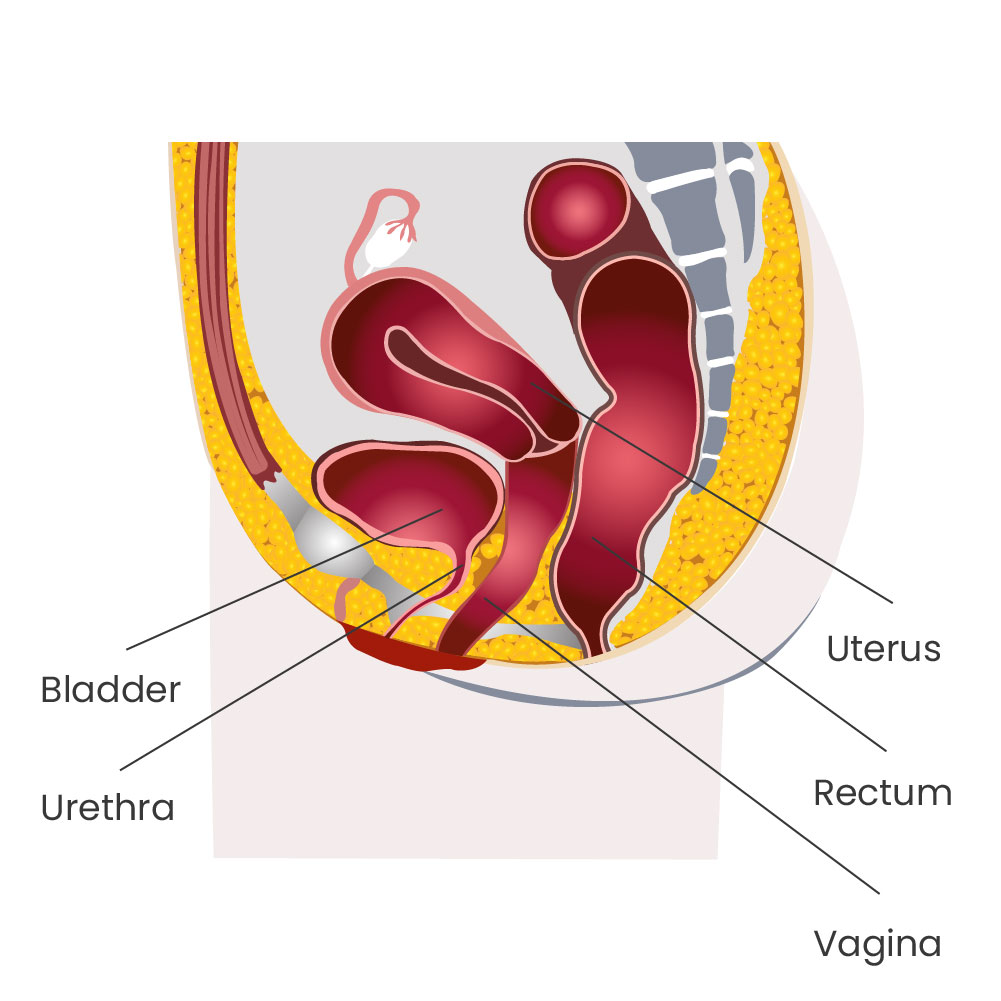
Types of prolapse include:
- Cystocele (bladder)
- Rectocele (rectum)
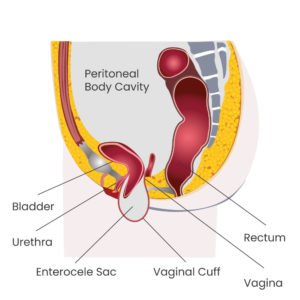
- Enterocele (intestine)
- Urethrocele (urethra)
- Uterine Prolapse (uterus)
- Cervical Prolapse (cervix)
If there is no uterus or cervix, vaginal prolapse is sometimes referred to as vaginal vault prolapse. All of these sub-types simply help to identify what is responsible for this bulge into the vagina (different names suggest different pelvic organs).
Vaginal prolapse, sometimes called pelvic organ prolapse (POP) is not typically dangerous, but can cause considerable discomfort and bothersome symptoms.
Vaginal Vault Prolapse Symptoms
Common symptoms for vaginal prolapse include:
- Feelings of pelvic pressure or fullness, pulling, or tugging (especially with heavy lifting)
- Feeling as if you're sitting on an egg or ball
- Seeing or feeling a bulge or ball at the vaginal opening
- Difficulty with vaginal intercourse
- Urinary frequency, urgency, or urinary incontinence
- Spraying with urination
- Difficulty with bowel movements
- Abnormal bleeding from the vaginal canal*
If you're having abnormal vaginal bleeding, please see your doctor for evaluation.
Vaginal Prolapse Diagnosis
Vaginal prolapse is diagnosed by your doctor or medical provider an internal and external pelvic exam. This exam often includes the use of a speculum. During the speculum exam, your doctor may ask you to bear down, push, or cough. These techniques help to make the prolapse more pronounced and can help identify which portion of the vagina is moving into or toward the vaginal opening.
The diagnosis of pelvic organ prolapse often includes staging using what is known as the POP-Q (pelvic organ prolapse quantification) staging system. This staging system rates the extent of prolapse on a scale of 0 to 4 (0 is no prolapse and 4 is complete prolapse).
The POP-Q staging system also provides specific measurements of the different compartments of the vagina. This allows clear communication from one medical provider to the next about the location of vaginal prolapse, which wall or walls of the vagina may be protruding, and by how much. It also lets your doctor monitor the progression (or improvement) of your vaginal prolapse over time.
Knowing the POP-Q stage is important for developing a treatment plan (whether surgical or non-surgical) and knowing the location of the vaginal prolapse is important as it can relate to the types of symptoms you may be having.
The location of the vaginal prolapse can allow your doctor to make informed decisions about how each of the various treatments may improve your vaginal prolapse symptoms.
Vaginal Prolapse Treatments
Treatment options for vaginal and pelvic organ prolapse encompass a wide array of surgical and non-surgical methods. At the Midwest Center for Pelvic Health in Indianapolis, we tend to talk about these treatment options with our patients as if they were on a spectrum from least invasive to most invasive.
Watch and Wait (Expectant Management)
Because vaginal prolapse is most often not dangerous, the least invasive treatment option is what’s known as “expectant management” – also called watching and waiting. This is a reasonable option for many women, especially if the prolapse causes no (or minimal) symptoms. It is important to note, however, that symptoms can get worse over time.
Home Exercises
As we continue to move down the continuum of treatment options, the next treatments include home exercises. These can involve what are commonly known as Kegel exercises — targeting the pelvic floor muscles. Oftentimes, Kegels alone are not enough. Many patients also require core strengthening and postural changes to gain relief from vaginal prolapse symptoms.
Pelvic Floor Physical Therapy
Many times these exercises of the pelvic floor muscles and core require the advice and consultation of a physical therapist who is specialized in treatment of pelvic floor disorders. Therapists are skilled in the evaluation and management of these disorders and can offer hands-on therapy, coaching, and support customized to your comfort level. There are many quality pelvic floor physical therapists in the Indianapolis area, and we would be happy to connect you with one of them.
Pessary
In addition to pelvic floor physical therapy to strengthen and repair the muscles and connective tissue of the pelvic floor, sometimes patients require the use of a vaginal support device called a pessary.
Pessaries are simply devices that are worn inside the vagina to push the walls of the vagina (and even the uterus) back into their normal position during day to day activities. When we discuss pessaries as a treatment option for women, they often have two questions:
In addition to pelvic floor physical therapy to strengthen and repair the muscles and connective tissue of the pelvic floor, sometimes patients require the use of a vaginal support device called a pessary.
Pessaries are simply devices that are worn inside the vagina to push the walls of the vagina (and even the uterus) back into their normal position during day to day activities. When we discuss pessaries as a treatment option for women, they often have two questions:
What does a pessary feel like?
A good fitting pessary should wear like a wristwatch or a pair of glasses. If you think about wearing those things, you know that they’re present. You don’t have to reach up and touch your glasses to know that you’re wearing them, but they are not uncomfortable — you typically can carry on your entire day without noticing they’re in place. The same is true for a pessary. A good fitting pessary should not be painful, uncomfortable, or bothersome on a day to day basis. They should be a relatively low-maintenance way to eliminate the vaginal bulge and avoid surgical risk.
What does a pessary feel like?
Pessaries can be managed by you (the patient) or by us in the office. Patients who manage their pessaries at home typically remove the device about once per week. Some women rinse and replace immediately and other women leave it out overnight or even for a couple of days (depending on planned levels of activity).
If your pessary is managed in the office, we typically see patients every three months for removal of the pessary, cleaning, and examination of the vaginal tissue. Your comfort level with self management, the type (shape and size) of pessary, and the preference of your medical provider will determine what pessary management plan is right for you.
Many patients do quite well with pessaries for a number of years. Others do not like the idea of wearing something in the vagina for a prolonged period of time and decide to pursue surgical options.
Surgery
Surgical options for vaginal prolapse also cover a wide range and can be divided into multiple categories. Some surgical procedures (called obliterative procedures) do not allow for future vaginal penetration or intercourse. Others preserve that function.
For most women, preservation of sexual function is desired. In fact, most women who have surgery for vaginal prolapse state that their sexual function is improved after surgery.
Determining Your Goals
When determining a plan for you, we will ask many questions to determine your goals (like sexual function) as planning for your surgery will be largely focused around these goals.
Questions to determine goals for surgery may include:
- Do you want the most durable repair?
- Do you want to avoid using grafts or mesh?
- What are your goals for timing of recovery?
- Does your job, lifestyle, or a hobby require continued lifting?
- What other medical problems might increase your surgical risk or prolong your recovery?
- What surgeries have you had in the past [that might increase your surgical risk]?
- Have you had a hysterectomy? Do you desire a hysterectomy?
- Do you have a family history of risk factors that would alter the surgery in any way?
All of these questions will help to inform our decisions about what surgical type best suits you and your particular goals.
In general, surgical repairs of vaginal prolapse that involve preservation of sexual function are divided into two main categories. Both of these approaches allow us to repair the vaginal prolapse and return the vaginal wall(s) to its normal location. With few exceptions, procedures to repair vaginal prolapse do not restore the normal structure or function of the pelvic muscles themselves.
Vaginal Repair
Vaginal repair of vaginal prolapse involves surgery completely performed through the vagina. During this surgery, the doctor will use your own connective tissues and ligaments (along with suture material or “stitches”) to recreate the normal vaginal support and restore the vagina to its normal position.
Laparoscopic Repair
The other type of surgery involves small (half-inch) laparoscopic incisions into the abdomen. Through those incisions we place a camera and small instruments that allow us to identify the vagina from the inside of the pelvis. We can then elevate and support the vagina using either your own tissues or vaginal grafts/mesh.
Conclusion
There are many types of vaginal prolapse. Conversations/examinations with and by your medical provider can help not only identify the type of vaginal prolapse you have, but also uncover the specific goals that you have for treatment.
The most important part of the work we do at the Midwest Center for Pelvic Health is centered around
- Determining your goals
- Educating you about the options
- Working with you to build and implement a customized plan to achieve these goals
If you suffer from these bothersome symptoms of vaginal prolapse, call or schedule an appointment today. Let’s start this conversation so that we can develop a treatment plan that gets you back on the road to feeling like your normal self.
